Explore the groundbreaking science behind our smoke-free journey
When it comes to science and research, we set ourselves the highest standards, and our scientific methods are inspired by the pharmaceutical industry. We share our scientific findings publicly and encourage others to review our work.
Our vision is to offer adult smokers who don’t quit a better choice than continued smoking, and to transform for good. How are we making this vision a reality? By developing and delivering a portfolio of better alternatives to smoking that provide nicotine without burning tobacco, and which adult smokers find satisfying.
Tobacco harm reduction
Assessing product health impacts

Assessing our product health impacts
Celebrating 10 years of smoke-free progress
Our “PMI: A Story of Innovation” video series takes a fascinating deep dive into the early days of our transformation, the successes we’ve achieved, and the problems we’ve overcome since launching our leading heated tobacco product a decade ago.
PMI: A story of innovation
It was a very interesting journey, a very exciting journey with frustrations
from time to time, with setbacks. But I think we did the right thing.
Music rises and graphics appear showing early designs and the evolution of PMI's heated tobacco products from 1990 to 2023.
Text shows title of video: PMI - A Story of Innovation - #05: Never Stop
Moira Gilchrist, Chief Communications Officer, PMI, sat in an office, speaking to camera:
Being there from the very, very beginning,
since it was just an idea that was sketched out on a flip chart to where we are now.
And that's, a sense of enormous pride at what we've done.
Shea Lih Goh, President, PMI Japan, speaks to camera:
Every function within the company has undergone some sort of transformation.
Lisa Hook, Member of the Board of Directors, PMI, speaks to camera:
It is extraordinary to get to be on this ride.
Video cuts to the PMI office building in Lausanne, Switzerland
André Calantzopoulos speaks:
I have never regretted for a second that we went into this product.
What I regret is we didn't have the knowledge and the understanding,
I can blame myself for that, to avoid certain of the difficulties and the problems we had in the initial years.
Jacek Olczak, CEO of PMI, sat in an office speaking to camera:
Knowledge of anything today and you go back in time, you could do things differently.
But the knowledge today is the result of
experiences you build over the last period.
Graphic shows human brain which changes to stacked cubes with text: Knowledge is the result of experiences you build.
Lisa Hook speaks:
There has never been a moment where the board or the management team
has hesitated to keep pushing forward.
Urs Bringold, VP Content & Owned Media, PMI, speaks:
There was once sort of a visual just to illustrate what one day we would have.
The illustration was: you saw a tobacconist shop and you had a side
that was like ‘cigarettes’ and on the other hand, you had ‘IQOS’ and all that.
And I swear it, a lot of people internally before it launched were like,
'It will never happen' and all that. And now it is, you know.
Graphic shows tobacconist shop and text to the left 'Cigarettes' and to the right 'Smoke-free products'.
Stefano Volpetti, President Smoke-free Inhalable Products & Chief Commercial Officer, PMI, speaks:
The only gift here would be the gift of all the learnings that we had in the last ten years,
have it as of day one. Because that would have accelerated this journey.
André Calantzopoulos speaks:
As executive of a company, you always say, 'If I knew when I started what I know when I finished,
that would be a very different company.'
Video cuts to the PMI office building in Lausanne.
Moira Gilchrist speaks:
So, where do we go from here?
I think now it's about continuing to build on the science.
It's about continuing to listen adults who smoke.
Serge Maeder, Global Head of RRP System Innovation, PMI, sat in open-plan office, speaking to camera:
We have just opened a small door, but I think we have a lot of options to make this product better.
But yes, you're talking to the wrong guy,
you’re to talking to the guy whose job is to improve the product going forward.
Mimi Kurniawan, Chief Diversity Officer, PMI, speaks:
What is the next product, what next innovation? What else?
Graphic shows early designs and the evolution of PMI's heated tobacco products from 1990 to 2023.
Text reads: What is the next product/innovation?
Karlygash Bismeldinova, AGC, Commercial Development Law, PMI, speaks to camera:
Never stop. And this is what I really like about PMI. We're always in the process of progress.
Emmanuel Babeau, CFO of PMI, speaking to camera:
Ten years ago, the level of skepticism, cynicism sometimes, on our ambition to unsmoke the world
and become a smoke-free company was very high.
Ten years after, I believe that nobody today can seriously challenge how genuine we are in delivering this ambition.
Graphic shows a cigarette broken in half and text: 10 years ago/after cynicism of our ambition
Graphic changes to a parcel box and text reads: Nobody today can challenge how genuine we are.
Serge Maeder speaks:
We have a chance, in the next 10 years to go full smoke-free products in PMI.
Stefano Volpetti speaks:
If you take Tokyo, more than 50% of the volume is in smoke-free products.
The direction is set.
Shea Lih Goh speaks:
I think today, as we said, we have many things to be proud of in Japan.
But we are not resting on our laurels. Obviously, we want to do more.
So, I'm very, very sure in the next 10 years, there will be a lot of significant achievements.
Jean-Claude Schneider, Global Head, New Business Opportunities, PMI, sat in open plan office, speaks to the camera:
Innovation is coming. I don't know what we're going to have maybe in three, four, five years.
But I know something is going to be available, that we're going to have a constant evolution.
Moira Gilchrist speaks:
We've made incredible progress, but there's a world still of a billion smokers.
So, we're kind of one smoker at a time.
Stefano Volpetti speaks:
We are sitting on something that can change the trajectory of public health.
Graphic appears showing a speedometer and text reads: Get there faster, help from stakeholders, health regulators
Stefano Volpetti voice over graphic:
We're going to get there faster if society, antis, stakeholders, health regulators help us to go in that direction,
but not because they need to help PMI,
but because we have a responsibility to consumers out there to provide them with better alternatives.
Video cuts to the PMI office building in Lausanne
Bin Li, Chief Product Officer, speaks:
Ten, 15 years ago, we said that, 'We may be able to do it, to replace cigarettes.
To give smokers a better alternative.'
Graphic appears showing a cigarette and an IQOS device.
Text reads: We may be able to replace cigarettes. Better alternative
Scott Coutts, Senior Vice President, Operations:
When we say we want to do something, we can change the industry as we're doing today.
Lisa Hook speaks:
I think it’s the most extraordinary achievement I've ever seen any corporation accomplish.
Mimi Kurniawan speaks:
This is showing that we are achieving the bold vision and the bold milestone that we set for ourselves.
Shea Lih Goh speaks:
I'm just proud to be part of this journey and this beautiful history.
Jacek Olczak speaks:
I have no regrets. There were a lot of hard days. But I have no regrets.
André Calantzopoulos speaks:
All these things have taken lot of time. But are important milestones in your filmography.
It's many happy endings, but still it's many episodes to come.
Jacek Olczak speaks:
This is a great movie. You don't want this movie to finish, I want to see more of this, more of this.
Video cuts to Moira Gilchrist sitting in a chair, filmed by a camera, writing on a notepad.
André Calantzopoulos sitting in a chair, being filmed by a camera crew member, asks:
Female voice behind camera:
Everyone happy? Yeah. Go.
André Calantzopoulos sitting in a chair, being filmed by camera crew members, asks:
What was your question?
Female voice behind camera:
Your proudest moment?
Bin Li sitting in a chair, being filmed by camera crew members, speaks:
Two words come to my mind.
Video shows Jean-Claude Schneider's notepad
Female voice behind camera speaks:
Lowest moment?
Jacek Olczak speaks:
Oh, lowest?
Female voice behind camera speaks:
Yeah.
Jacek Olczak speaks:
You know me very well, I am a born optimist, okay.
Mimi Kurniawan speaks:
Sorry. I changed.
Video shows Karlygash Bismeldinova's notepad.
Karlygash Bismeldinova speaks:
Future is always difficult.
André Calantzopoulos speaks:
What was the toughest moment?
Video shows Lisa Hook's notepad.
Lisa Hook speaks:
Can you give me some ideas?
Jean-Claude Schneider speaks:
That was simple.
Video shows Scott Coutts's notepad.
Scott Coutts speaks:
Our hope for the future.
Shea Lih Goh speaks:
Full name?
Video shows Stefano Volpetti's notepad. Male voice behind camera speaks:
That's wonderful handwriting.
Stefano Volpetti speaks:
Wonderful or terrible?
Urs Bringold speaks:
Oh, no. I have to take a new...
Bin Li speaks:
Do I sign?
Jacek Olczak speaks:
You ready?
Video shows graphics of everyone's notes from their notepads alongside a short video of them writing in their notepads in the following order:
Jacek Olczak, Mimi Kurniawan, Moira Gilchrist, André Calantzopoulos, Jean-Claude Schneider, Shea Lih Goh, Bin Li, Serge Maeder.
Graphic appears: PMI A story of innovation
Jacek Olczak speaks:
I think we did the right thing.
Philip Morris International logo appears with text underneath reading: The End!
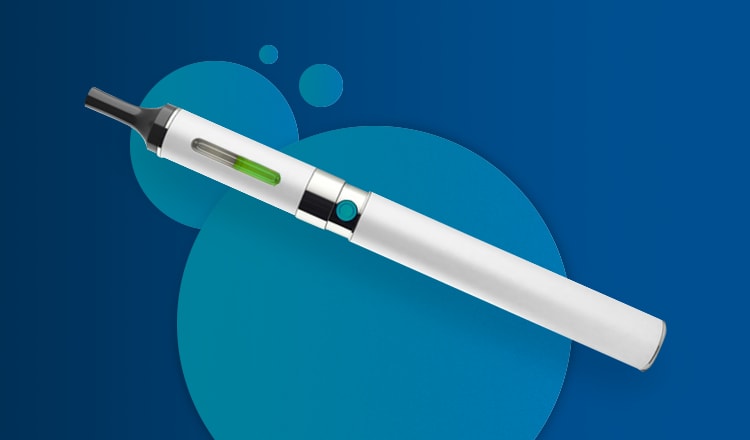
All about: Heated tobacco products